by Denise M. Dudzinski, PhD MTS
In March of 2016 AJOB published an article, Bioethicists Can and Should Contribute to Addressing Racism. Authors Danis, Wilson, and White wrote, “This commitment [to justice] is manifest in an obligation to promote health equity – to ensure that all people have full and equal access to opportunities that enable them to lead healthy lives. Differences in health that are avoidable, unfair, and unjust represent inequitable health. As such, the discipline of bioethics has at its core mission a mandate to pay attention to and help address social injustices affecting African Americans.” The authors are right. Now how do we do it?
Many white bioethicists like myself have sidestepped robust engagement with systemic racism. Having not experienced racism first-hand, we have the privilege of ignoring it if we choose. However, the more I learn about the social determinants of health, structural racism, and implicit bias, the less complacent I become.
Structural racism is embedded in the legal and social scaffolding of our country. Some elected officials are devoted to eradicating racist policies, practices, and attitudes while others rely on structural racism to further segregate and marginalize people of color. Since the 2016 presidential election, racist policies and proclivities, previously cloaked in euphemism and coded in shame, are openly endorsed. What role should white bioethicists play in resisting this disturbing turn?
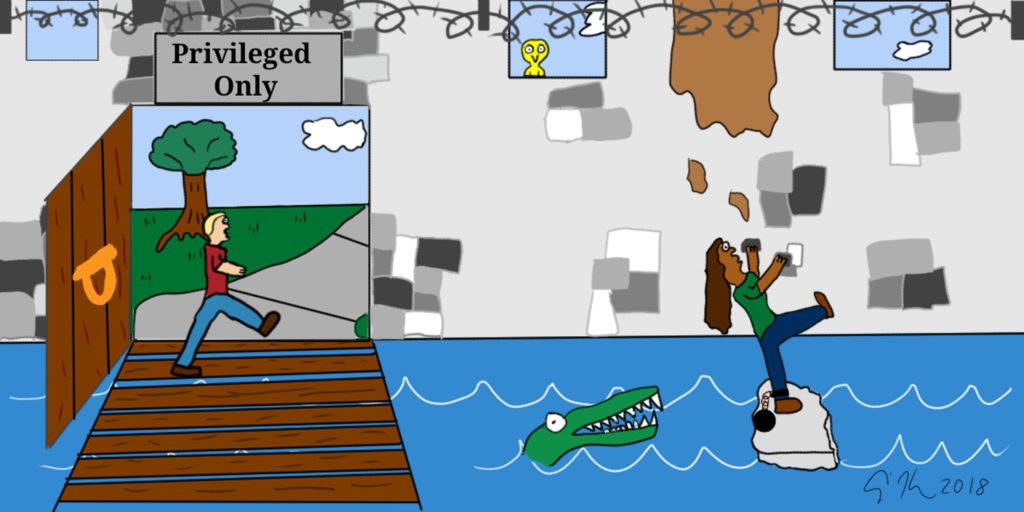
We can start by acknowledging white privilege. White privilege is “unearned power conferred systematically”. Whites are given the benefit of the doubt. Our motives for being somewhere do not bear undue scrutiny from strangers or law enforcement. Deference is paid to us & fewer obstacles arise in our efforts to exercise our rights, pursue our goals, and hold positions of authority. The privilege is marked by its invisibility to those who enjoy it and its conspicuousness to those who do not. Whites may take our independence and freedom for granted because we have known no differently. White privilege gives white people the option of playing it safe – of not speaking up or taking risks if we do not want to. Our colleagues, students, and neighbors of color do not have this option.
White bioethicists, who comprise the majority of bioethicists, are faced with a choice. We can ignore or dismiss white privilege or we can own it so it that it does not own us. I regret the many years I neglected to take responsibility for my part in systemic racism by, among other things, failing to appreciate white privilege’s impact on people of color.
“White guilt” helps us play it safe. The crimes of our ancestors and our complicity in subsequent oppression provoke guilt. White privilege creates the myth that our guilt is an undue burden. Upon reflection, this belief is deeply offensive. Our friends, colleagues, and neighbors of color are subjected to racism, which is indisputably painful and harmful. They are simultaneously expected to combat it – often alone. This is unfair and unreasonable.
White bioethicists can step into white guilt and accept that grappling with it is an important part of the work we do. Like many white colleagues, I worry about offending, overstepping, being insensitive, racist, and naïve. Inevitably these worries will come true, but my friends and colleagues of color have always met these offenses with forgiveness, patience, and a willingness to teach. I acknowledge that asking minority colleagues to instruct me is yet another burden, but the alternative — whites making assumptions about the experiences of minorities — is worse, so I am grateful for their help.
So exactly what are white bioethicists’ responsibilities? As a clinical ethicist, I have quite a few. The Code of Healthcare Ethics Consultants (HCEC) says one of my responsibilities is to “promote just health care within HCEC. HCE consultants should work with other healthcare professionals to reduce disparities, discrimination, and inequities when providing consultations.” Clinical ethicists do this in a variety of ways: by identifying “avoidable, unfair, and unjust conditions” operating in the ethics consultation, including our own biases related to race or poverty. We unpack comments about the ‘difficulties’ of caring for minority patients, because clinical jargon sometimes sanitizes and legitimizes racial bias. We also acknowledge our shared humanity — that all people, including ethicists and health care providers, hold negative biases but we do not excuse them. We can name racial bias without euphemism, with kindness and a sense of solidarity in our collective efforts to stop hurting people of color. We enlist our clinical colleagues to find ways to curtail the harm racism causes our patients, their families, and staff. We write and enforce policies that acknowledge and address bias. We work on this every day, together.
As a professor who teaches healthcare professionals, I talk openly about implicit bias with my students and no longer save the discussion for justice talks. When discussing a clinical case or policy, I no longer raise the question of whether implicit bias – racial or otherwise — is a factor. I ask how it is a factor. It occurs to me that those who have never been subjected to racism have the luxury of asking ‘whether’ racial bias is relevant. Race is always relevant to those who confront racism every day. It may not be the focus of our ethical analysis in a particular case, but systemic injustices are ethically relevant, and my job as a bioethicist is to name them and help my students understand and resist them.
I want to stop playing it safe, resting comfortably in white privilege. I also want to thank those bioethicists who had this revelation long ago, many of whom have been writing about racial injustices for years. This post is for the rest of us.