 It is important for everyone to understand that in the 50-year history of brain death, going back to the Harvard Criteria of 1968, no patients determined to be brain dead by generally accepted guidelines have ever become undead. There has never been resumption of spontaneous breathing, re-emergence of brainstem reflexes (pupillary, eye movement, corneal, gag, or cough reflexes), or recovery of responsiveness other than spinal reflexes.
It is important for everyone to understand that in the 50-year history of brain death, going back to the Harvard Criteria of 1968, no patients determined to be brain dead by generally accepted guidelines have ever become undead. There has never been resumption of spontaneous breathing, re-emergence of brainstem reflexes (pupillary, eye movement, corneal, gag, or cough reflexes), or recovery of responsiveness other than spinal reflexes.A Few Words on the Saga of Jahi McMath
by James Zisfein, MD
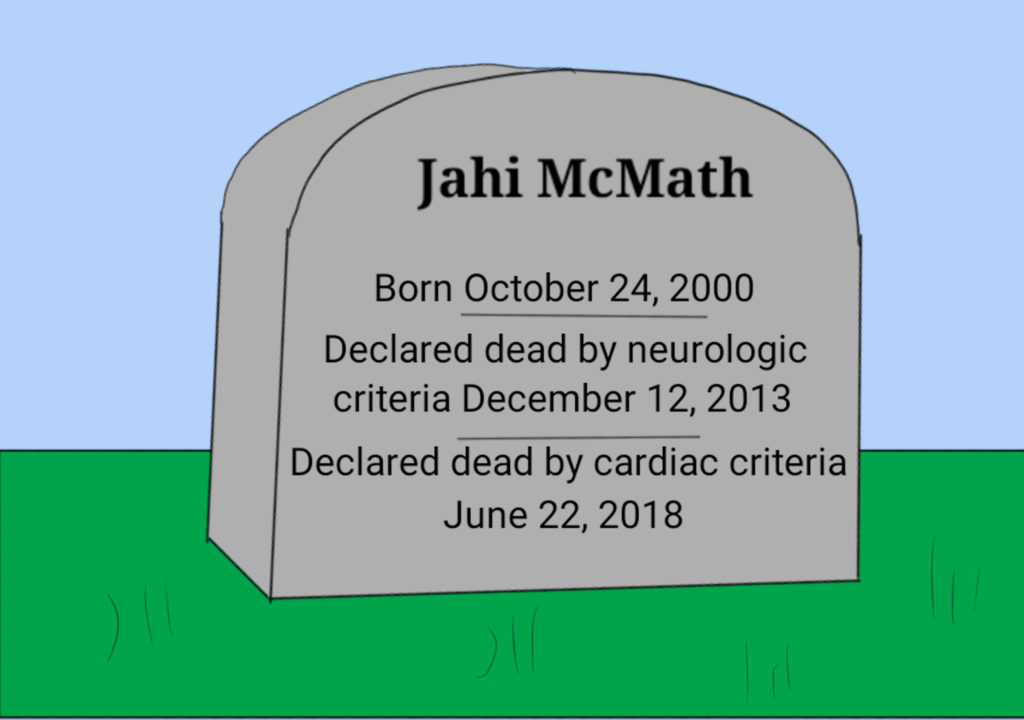
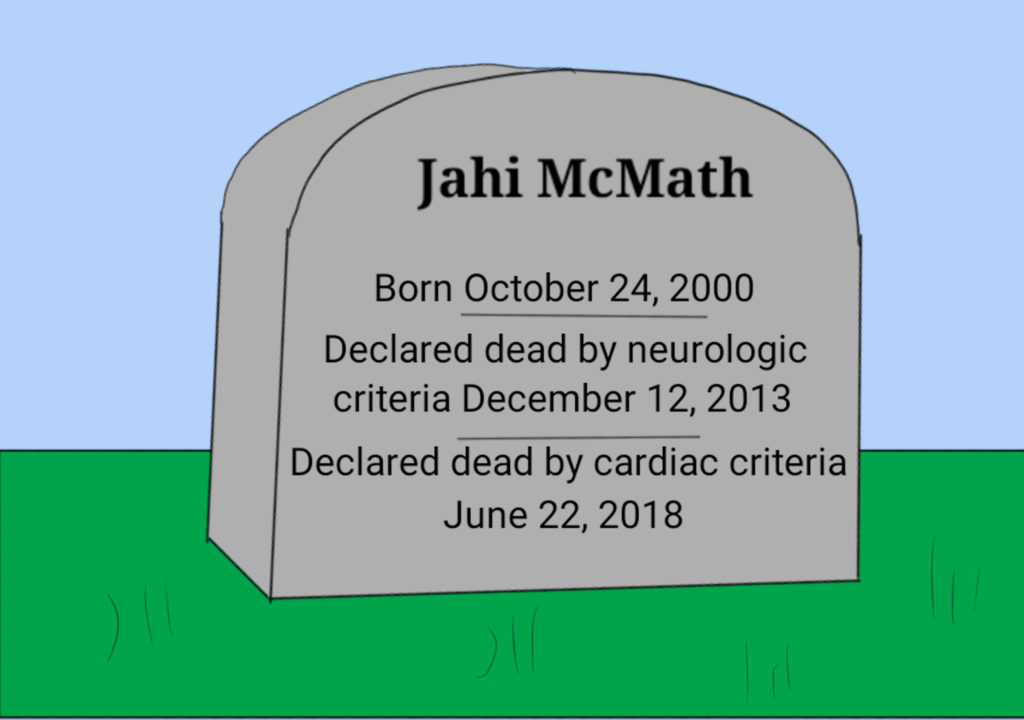
A few words on the saga of Jahi McMath, the teenager who became brain dead from a surgical complication, whose family refused to accept that determination, and whose heart has stopped and is now dead by everyone’s definition:
The fact of McMath’s death over 4 years ago should not be in question. The original determination of death at Oakland Children’s Hospital was in full compliance with published medical standards. Several physicians confirmed that determination. There have been no subsequent neurologic examinations of McMath demonstrating evidence of life.
Alan Shewmon, a neurologist called in by the family, expressed his belief that McMath was responsive based on videos that showed finger movements after she was instructed to move her fingers. However, since the response to instructions was not reproducible and were also finger movements without instructions, a more reasonable interpretation would have been that the movements were spontaneous and not responsive.
 It is important for everyone to understand that in the 50-year history of brain death, going back to the Harvard Criteria of 1968, no patients determined to be brain dead by generally accepted guidelines have ever become undead. There has never been resumption of spontaneous breathing, re-emergence of brainstem reflexes (pupillary, eye movement, corneal, gag, or cough reflexes), or recovery of responsiveness other than spinal reflexes.
It is important for everyone to understand that in the 50-year history of brain death, going back to the Harvard Criteria of 1968, no patients determined to be brain dead by generally accepted guidelines have ever become undead. There has never been resumption of spontaneous breathing, re-emergence of brainstem reflexes (pupillary, eye movement, corneal, gag, or cough reflexes), or recovery of responsiveness other than spinal reflexes.McMath was not an exception.
McMath reminds us that when a brain dead patient is maintained on medical support there can be preservation of some bodily functions. The heart can continue beating. Blood pressure can be maintained. The kidneys can make urine. The gut can process tube-fed nutrients. The liver can metabolize endogenous and exogenous substances. With hormonal support, a pregnancy can progress to term, a child can go through puberty, and menstruation might occur. It is possible that the part of the hypothalamus that supports pituitary function can remain active in brain death. That would violate the Uniform Determination of Death Act (UDDA) requirement that there be no function in the “entire” brain, but it would not violate current medical guidelines. If anything needs fixing here, it’s the UDDA.
Whether brain death is truly biological death is unknown and I maintain that it is unknowable. Brain death is not a naturally occurring condition and does not observe natural rules of life and death. Brain dead patients have some features of life and some features of death. In the absence of biologic certainty, death becomes a matter of consensus and ultimately a matter of law. And the law (at least in 49 states, New Jersey is the outlier) is clear: brain death is death.
McMath was a disaster, most of all for her family. I’m not just referring to the catastrophic event that caused her death, but to the subsequent years of agony that were entirely preventable. It’s part of the job of bioethicists to prevent disasters.