by Craig Klugman, Ph.D.
Last week, I was interviewed by an academic news serviceabout antimicrobial resistance (AMR) after a study reported that giving antibiotics to children in selected African towns led to a decreased mortality rate. The reporter learned of my work by reading the blog I had written on AMR a few weeks before. Many reporters today will send a list of questions to which you can write answers. Sometimes they will speak you to after you’ve read the questions and other times they will accept written answers. I find these approaches better than a cold phone interview because it allows me time to think more carefully about what I have to say and to be sure that the words accurately reflect my thinking.
As I sat down with the list of questions, I found myself thinking from a variety of perspectives. Although I had two hours to respond, I found myself writing, deleting, and rewriting over most of that time. In part, you want the words to send more like a dialogue than like formal writing. And second, I realized I was not offering a coherent message, but one that varied depending on how I was analyzing the article. I thought about the study while wearing a variety of different hats.
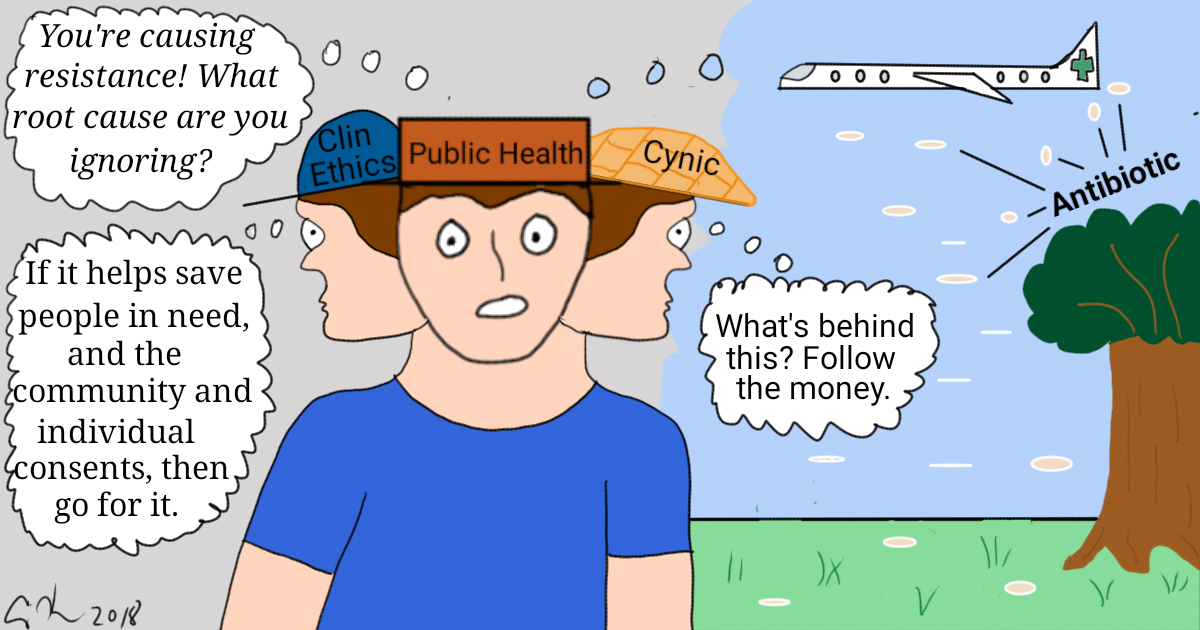
For instance, while wearing my Public Health Ethics (PHE) hat, I was horrified at this experiment. I immediately looked to see what IRB would approve this (several as it turned out). I wrote about the need to make sure that we preserve the effectiveness of antibiotics for future generations. Thus, my perspective was that we should triage their use today because intergenerational justice said we owed efficacy to tomorrow. My PHE self was appalled at the idea of just giving out antibiotics to a large group of people (in this case, single large doses every 6 months) because such an approach creates the conditions that select for resistance. I also asked what this approach masked: Were there underlying, undiagnosed diseases that we could learn to identify more easily so that the response could be targeted and provide less evolutionary pressure on the bacterial population as a whole. After all, giving a drug to an entire community is a hammer approach to trying to fix a screw. Wouldn’t it be better to find the right tool to the specific problem?
This perspective also led me to write about the ecological fallacy—just because this approach seemed to change death rates for a population does not mean that antibiotics given to a particular individual would improve their chances of living—and confounding variables—what else was going on in the villages at the time that might have changed the death rate.
Under my clinical ethics hat, I was intrigued that there was a simple and not terribly expensive way to decrease deaths. I began by thinking about individual and community autonomy. Did the key stakeholders (i.e. mostly community leaders) consent to this experiment? Did the children’s parents consent? The answer to both of these questions was yes. If the approach was with consent (autonomy); the benefits (beneficence) were proven and outweighed the risks (nonmaleficence; beneficence); and the program was affordable and available to all (justice), then we should do it. Putting principlism aside, would a deontologist see a duty to help save the lives of children with an inexpensive and effective intervention: Yes, and the consequences of AMR would not even be a factor for consideration. A utilitarian would see saving many lives of a community today as a higher pleasure than saving unknown and perhaps not-yet-existing lives tomorrow (especially via Act Utilitarianism). Overall, if there are patients in need standing before us, then we should provide assistance to them.
Lastly, I put on my cynical hat. Why was this particular antibiotic chosen? Why this particular approach? I looked at the grant application on the federal website and more carefully read the article. The study was funded by the Bill & Melinda Gates Foundation’s global health initiative: “Our Global Health division seeks innovative, ambitious, and scalable solutions to address health problems that have a major impact in developing countries.” What I did not find was who paid for the antibiotics? The foundation? Did a company donate them? Who stands to gain, financially, from a sudden increase in sales of this antibiotic? The drug costs $0.47 to $77.12 per package depending on the source. There is one manufacturer that is larger than all of the others: Would it benefit?
I wrote 3 pages, discussing the issue from these various viewpoints and then deleted it. Sometimes a report wants you to help them think about the issue (often early on in the story and usually does not get you a mention in the piece) and other times they are looking for a quote from a particular perspective. Knowing that the reporter had read my blog, I knew that I had to offer commentary from that place. I simplified what I wrote, trying to keep to no more than 1 page. And rather than be all over the place, I chose a stronger perspective (PHE) from which to speak. Given that this was a science news source, I knew they would be more interested in the nuance than a lay news organization. Thus, I could go to one page whereas normally I would keep my response shorter. In these longer explanations, I try to “help” the writer by highlighting (in bold) what I think are the best key phrases that might be helpful. In an oral interview, the same approach can be achieved by pausing before and after you speak the words that you think make a good quote. This is a way to guiding them to what you think are the best quotes, but also giving them a fuller explanation of the issue.
Once you send the answers to a reporter, they and their editor pick and choose what sections they will use as quotes in the article. Thus, once you send off your words, how they are represented are out of your control. For this particular article, the author was interested in my comments on intergenerational justice and my brief description of the cause and effect of antimicrobial resistance. When I posted on social media, the (not so positive) comments ran the gamut of the various thoughts I had when wearing multiple hats: It’s about saving lives, not ethics; what about when the researchers leave and take their drugs with them; how do you tell the mother whose child is dying that she can’t get the drugs because some future patient might need it more? I agreed with all of the respondents’ comments and with none of them depending on which hat I put on. Scholars in bioethics are disciplinary polyglots, speaking with different methods and varied analytical perspectives. But at the end, we have to make a recommendation or provide a quote, and that requires us taking a stance (even if that stance is merely which analysis to favor).
Offering a bioethics commentary or analysis on a study or a case is a multifactorial process that draws from our many experiences and our varied training. But when you are represented as only a single quote or two, that deep description is lost. That’s why I try to provide explanations and highlighted keys to the main quotes and ideas to the report. And that’s why I wrote this blog, to bring back the depth in my analysis that could not be represented in a news piece; and to show that I was simultaneously intrigued and horrified at it. This is the power of a bioethics perspectives and the challenge of sharing that with the world. Both analysis and sharing, however, are our professional duty.